Treating tinnitus and visual snow with rTMS
Trying magnetic stimulation to reduce network brain activity
You know the list by now — I hear cicadas in my ears all day long, and I can’t look at a beautiful scene without being overwhelmed by the brightness of very ordinary light. Without light-blocking glasses, I see static everywhere and my limbs lose sensation. Headlights and overhead lights look like a cluster of blazing suns. I sometimes have an internal tremor that makes me feel like I’m vibrating. Grrr.
What to do about this? Not much, I’m told. The mainstream medical approach is “habituation.” Get used to it. Ignore it. Sometimes hearing aids help, or tinted lenses and eye retraining exercises. To cope, I often listen to music, podcasts, or the sound of rain. I’ve got the glasses. I’ve adjusted somewhat to this new reality, but at certain points of the day, I can’t even pretend to be moderately comfortable. I’ve had kidney stones, among the worst kinds of pain, and this is often up there in terms of discomfort. I long for the ability to see and hear as I once did—to experience peace instead of punishment just for being conscious—and I wonder if I will ever have that again.
In my endless search to turn over every stone, I found rTMS protocols that deliver significant relief to people with these symptoms. Finding a way to get care and the right diagnostic, however, is a whole other problem. Especially in this place.
This cluster of symptoms has a name: visual snow syndrome (VSS).1 I don’t get the honour of a diagnosis because my problems were induced by a chemical rather than a hit to the head or some other spontaneous event. I don’t care for diagnoses, but doctors seem to need them to direct care.
Up until recently, VSS has often been dismissed as psycho-somatic hysteria, but with uniformity of symptoms among sufferers, the medical system now sees VSS as a very real thing.
In the last post, I described the process of working on meta-level brain-body systems. In contrast, these particular problems require a very targeted set of brain interventions.
Protocols to try
Here’s the menu of rTMS protocols to target certain brain networks:
the auditory cortex for tinnitus
the temporoparietal junction (TPJ) for tinnitus and chronic pain
the dorsomedial prefrontal cortex for tinnitus and PTSD
the lingual gyrus for visual snow
the visual cortex for visual snow
the visual cortex for photophobia
Where should I start?
Tinnitus is something that bothers me constantly, and my visual snow and photophobia can be at least partly controlled with lenses and light settings. Two meta-studies on rTMS for tinnitus—that is, two systemic reviews of all published literature on it—indicate that rTMS has proven effective in suppressing tinnitus. So tinnitus seems like a pretty solid bet for the first protocol. I’ll focus on that here, and then follow up with a post on visual protocols.
Which tinnitus protocol works best?
The two meta-studies each reached distinct conclusions:
Target the auditory cortex (AC). The analysis done in November 2021 (of 29 studies) suggests that the protocol targeting the auditory cortex (AC) is the most successful;
Target the temporoparietal junction (TPJ). Another study published earlier that year (of 20 studies) identified that TPJ stimulation reported significant suppression.2 This study also concluded that only 50% of studies targeting the auditory cortex (3/6 cases) were successful.
One of the very useful outcomes of the meta-analysis is that they’re also learning more about what causes tinnitus in the brain through trial-and-error.
So, to help me decide which region to target, I sought to better understand what neuroscientists think causes tinnitus.
Neurobiological models of tinnitus in the brain
If you were to ask a lay person what causes tinnitus, they’d probably say that it’s an “ear” issue, and that exposure to loud noise created the problem in the first place. This is one model of tinnitus, specifically that “neural changes… occur between inner hair cells and the auditory nerve.”
This is a contributing factor for some folks, but for me, this isn’t the case. I had comparatively minimal tinnitus prior to the injury, but the noise escalated profoundly within hours of medication withdrawal. I had my hearing tested, too, and there’s no loss. So some brain network has been disrupted instead.
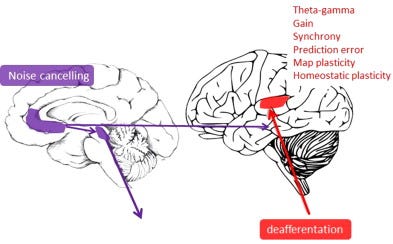
This leads us to the second idea: that tinnitus is primarily a “brain” issue. A number of brain regions are jointly activated in a series of subnetworks. Communication between brain regions occurs at certain “hubs” in the brain. If we find the right “hub,” the theory goes, maybe you can turn down the volume by changing the electrical frequency of the subnetwork.
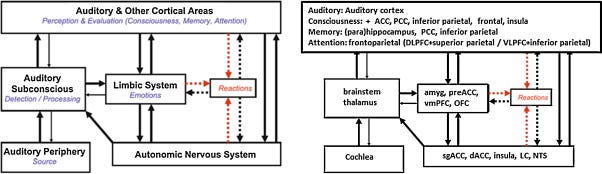
Here’s what the overall hearing network looks like in the brain:
Tinnitus starts in deeper brain structures and then reaches higher cortical areas, and that’s how it becomes perceived by the sufferer. It’s then classified as important by our internal filing system, and it goes unsuppressed. Finally, extra feedback is sent back to limbic structures (the deeper ones responsible for fight/flight responses). This creates a loop of perception and limbic activation. It is often experienced by folks with PTSD.
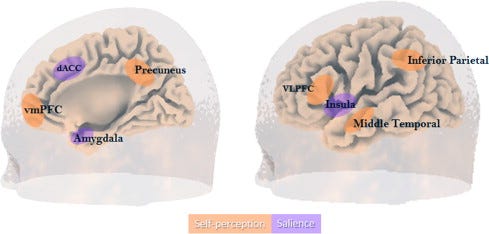
Tinnitus requires the activation of at least two primary brain networks: the self-perceptual network (self-explanatory), and the salience network (the network that prioritizes things as “important”).
The self-perceptual network is implicated because the noise is perceived by the sufferer as “external.” This network includes:
the anterior cingulate (ACC)
ventromedial prefrontal cortex (vmPFC)
ventrolateral prefrontal cortex (vlPFC)
the middle temporal and inferior parietal cortices (TPJ?)
The salience network prioritizes the sound as “important.” The critical parts of this network include:
the anterior cingulate cortex (ACC)
insula
several deeper brain structures (amygdala, thalamus, periaqueductal grey, and hypothalamus).
Imaging studies have determined that the ACC and insula are especially important for detecting a sound, and they’re also important for detecting “somatosensory” inputs (ie. paresthesia). These two brain regions are very relevant to my situation. Other imaging studies have found that chronic tinnitus is related to connectivity between the auditory cortex, insula, and ACC.3
Of note here, I infer—the TPJ appears to be implicated in part of the “self-perception” network, though I have not found a study that confirms this. Generally, the left TPJ is involved in connecting external symbols to existing knowledge and memories.
So, which hub should I target first?
It’s clear that multiple networks and hubs are involved in various aspects of tinnitus (loudness, chronicity, pitch, etc). But is there a “best guess” for a target hub? And if so, what frequency would change the connectivity?
I went back to one of the meta-analyses to see whether rTMS outcomes confirm or reject the proposed target areas (TPJ or AC).
The more detailed meta-analysis suggests that the AC is the best place to target, but not just because it reduces activity in the AC itself because it modulates activity in the insula. This observation supports the theory that tinnitus is related to impaired auditory information processing. An fMRI study also found more functional connectivity between the AC and insula for sufferers.
What does the insula do? It boosts “sensorimotor, pain, and socio-emotional processes to high-level attention.” Further, they write, “insular lesions can cause hyperacusis [sensitivity to sound] and central auditory deficits… direct electrical stimulation of the insula can induce auditory illusions and distortions.”
Tinnitus suppression of the AC tended to last at least 6 months.
The TPJ target, by contrast, elicited “the strongest electric field… in the cerebellum,” which is not a key region in any of the neurobiological models of tinnitus. Duly noted.
I also had one more look at the single study targeting the vmPFC (ventromedial prefrontal cortex), because it was also referenced in DeRidder study as a noise-cancelling hub.
In the vmPFC case, suppression was also sustained using excitatory (10 hz stimulation) five times a week over four weeks. I have other curiosities about this hub, though—the vmPFC is a noise-cancelling hub for fear centres in the brain, too, including the amygdala, which has become hyperactive as a result of this whole mess. The vmPFC is known to be less active for folks with PTSD, even though the hub also has the capability to alter the original fear and “override it with safe memories.” Excitatory stimulation of this hub may also improve social relating; at least it has done so for folks with autism.
Since the vmPFC protocol isn’t as well known, I suppose I should start with the inhibitory AC protocol, but I’ll keep this lesser-known protocol in mind as a possibility in the future.
Postlude: would it make sense to have a look at what’s going on in there?
All of this theorizing about brain hubs has me thinking: is there any way for me to have a detailed look at what’s happening in there? What might it look like on a map? Can I give the map to my rTMS provider?
The EEG that was done months ago yielded no results, or at least no information or feedback. fMRI scans are popularly used to study brain connectivity, and more recently, Dr. Daniel Amen has started to reliably use SPECT scans (single photon emission computed tomography) as a tool to evaluate bloodflow in the brain, and understand associated disorders.
In his book, The End of Mental Illness, not to mention a number of articles like this one, Amen argues that SPECT scans are underutilized, especially for folks with complex conditions (mine?), and that they can accurately transform “mental health care,” which involves a lot of stigma and guesswork, into “brain health care,” with a physiological root. Another biohacking site suggests that a SPECT might be the best way to uncover the source of internal tremors — in their case, inflammation in the thalamus.
I’ve spent a lot of time learning about what might be going on, and I’ve had to swim through a lot of stigma and guesswork, too. At least I know the starting point for me was a brain injury.

Would a SPECT scan even show anything related to tinnitus?
I found one study that used an MRI/SPECT fusion to identify abnormal blood flow for tinnitus sufferers. They identified higher bloodflow to the “secondary auditory cortex and associative cortex.” There were even more abnormalities in younger patients relating to “cognitive and emotional” changes, which likely demonstrates a heightened experience of stress and anxiety. This study also seems to confirm that the AC is the best place for me to start with.
So we’ve got a plan for the next couple of weeks: try to reduce the electrical frequency of my self-perception and salience networks. We’re going to try 5 sessions of the TPJ; 5 more of the auditory cortex/insula. That might reduce irritation for at least six months, while I seek other treatments — including a novel oxytocin spray that has been successful in the treatment of tinnitus.
Since my research into SPECT, I’ve taken the initiative to engage Amen Clinics to read a SPECT scan of my own brain, which I hope to undertake somewhere closer to home. The closest Amen Clinic is in Chicago. I seem to have found a willing scanner in Fargo, just across the border, but I’m just waiting on a referral from my family doctor. Shouldn’t be hard — I couldn’t even do a SPECT scan in Winnipeg if I wanted to!
All this research is so leading-edge and unusual that my doctors look at me sideways: they think I’m either brilliant or insane for setting this all up. I’m sure that if they were experiencing something even as moderately uncomfortable, they’d be calling in favours from their friends. The logic, however, does seem to prove itself, and the difference it could make to my quality of life is huge. I already found my first rTMS protocol to be life-altering, so I have hope that future rounds could be just as promising.
[post-treatment update: two protocols and some “cuddle spray”]
I had five sessions targeting the TPJ, and five sessions targeting the auditory cortex. During the TPJ sessions, I seemed to have very little tinnitus in the mornings, though I had the usual spikes throughout the day.
The AC target was obstructed by a nerve in my head, so my shoulder and face would convulse and they had to find a special angle for me. During this second phase of the treatment, I felt that I had some additional unusual spikes and headaches, though the quieter mornings seem to have endured.
Since the protocol began, I discovered another novel therapy for tinnitus: oxytocin spray, which is usually used to induce labour. In 2017, researchers from Brazil tested a high dose of the spray on suffers over ten weeks, and the initial results were promising. There is another major study being undertaken on the spray now, and pending those results, I’ve got a prescription on the way.
White et al explain that “numerous other non-visual or even non-perceptual symptoms have been identified,” for VSS, “including migraine, tinnitus, vestibular disturbance (consistent with persistent perceptual postural disorder), fibromyalgia, migratory paresthesia, and endogenous perceptual phenomena such as depersonalization and derealization.”
Specifically, TPJ targeting between T3-P3 or T4-P4 (6 cases).
My first rTMS intervention should likely have reduced the activation of the ACC, insula, and amydgala through the prefrontal cortex. My PoNS machine also sends signals up the periaqueductal grey. But these interventions clearly had very little effect on tinnitus.