Professionals on the Verge of AI-Induced Obsolescence
Three Moments on the Slow Automation Toward AI
Over the past two weeks, I’ve had three distinct encounters—each small but quietly damning—that reveal the deeper reason why so many credentialed professionals, especially in healthcare, are losing their grip on relevance at lightning speed (yes, a hell of a time to be a university professor!). None of these humans are unintelligent or ill-intentioned, but, as the ones at the top of the economic food pyramid, they operate as high-priced gatekeepers within systems that reward prohibition over problem-solving. AI will not replace them out of brilliance, but because its reasoning simply outwits incentivized atrophy.
1. The Disappearing Clinician
The first encounter was with a sharp, capable clinician—engaged, efficient, warm and seemingly invested in what was happening to me [therefore exorbitantly priced — you pay for that]. And then… nothing. No follow-up. No notes. No referral. No closure. Just disappearance. Like a radio signal that cuts out mid-broadcast, she was there, on paid time, then gone. She might come back eventually, but until then, the system absorbed her without a trace.
I doubt that I was ghosted, but I might have been abandoned. I suppose that’s the problem, it’s usually a procedural disappearance — in a private clinic, maybe life got in the way, or she’s on semi-perma holiday?
A decent AI would have at least feigned care in the aftermath and you wouldn’t have worried about paying for it. Humans are capable of doing that too, but in this system, they’re only rewarded for “moving on” and cramming in more (post-theft) for another round with a smile, rather than seeing anything through. It’s happened dozens of times — meanwhile, tests are misplaced, you’re given the runaround— you name it, this is commonplace healthcare.
2. The Pricing Oracle
The second was with a pharmacy technician. Again, professional, and probably good enough at his job. And yet, he’s bound to a Byzantine pricing algorithm that charged me $1000 for the same drug I had paid $27 for a couple of years ago. No clear explanation—just a labyrinthine new set of rules he can’t comment on, randomly invoked in the province of BC because… safety. Guidelines? I left it for a couple of days and did some of my own fruitless research about it… then when I asked for some more specific clarity to seek a solution, a huffy burst of confrontation came firing out, ending with something like “Are you confused? Do you need me to write it down?” [Except I had no explanation why this happened or what exactly I needed to do. That’s gaslighting, not confusion!]. At least a logic engine would have offered consistency, maybe a workaround, and likely wouldn’t have descended into condescending madness on their own treadmill of frustration.
They are features of a system that has become structurally antagonistic to anyone with ongoing, complex health needs. The only people who survive it—who actually get care—are insiders, or those adept at gaming the system. Those are people who know which code to use, which form to fake, which symptoms to underplay or exaggerate. How the rules might punish them in the process. Usually, that means doctors and medical practitioners themselves. For acute problems, this system might be more likely to help. For chronic illness, it is a labyrinth that moves its walls when you think you’ve found an exit and then blames you for failing to navigate it. A moral failure for being sick, on repeat — how utterly, quietly life-destroying for so many people.
3. The Missing Specialist
To get the kind of care I’m supposedly entitled to here in Canada, I’d have to see a neurologist or, better, a specialist in neuroimmune disorders. But such a specialist hasn’t existed in my province for at least five years. Meanwhile, generalist doctors acknowledge this absence [sheesh, how terrible, they feign] —but then they still require you to consult the hypothetical [read: fictional, nonexistent] specialist, if you ever get access, before dispensing the medications or rehabilitative procedures that allow you to function. They might shrug before blame-shifting [read: victim-blaming], and geez, your case is confusing [read: eyeroll, some part of this is your fault!] and hurry up my time is valuable! […notes in chart…]
So when you get tired of all that human procedural failure on a routine basis and try to find healing through other channels— private pay, compounding pharmacies, or (god forbid) efficient and well-priced international options—you’re met with disappearing acts, fines, forms, or silence. Or even a stern warning letter from the Canadian Border Services Agency who know better than you do and also require you to access the fictional doctor in this endlessly broken system. Or else they might just escalate the case next time. The system can’t possibly acknowledge how dysfunctional it is. Theatrical comedy-of-errors cruelty, anyone?
The care is in your best interest [he said, jokingly] but in practice, especially in Canada, that care is a government-paid refusal with a smile. You’re denied what you need while being told that your need is unreasonable. In this situation, what we call care in this country is a high-priced, well-paid “Dr. No” whose primary concern is to reduce healthcare costs to the payor unless they have to actually stop the visible bleeding somewhere. Which, I’m told, they do well.
The result is a revolving door of obfuscation, condescension, and stalled treatment with no capacity for problem-solving of the kind I’ve been able to successfully do on my own. It’s bureaucratic gaslighting that nudges you into either exhaustion, rage, or fits of laughter at the sheer futility of it all.
The Labyrinth, and the Lie
The worst part is the biggest lie of all, which is framing this obstruction as benevolence, and, if we want to ratchet up the irony, celebrating this as our single greatest national asset. A proud Canadian differentiator. But the delay, the denial, the “need to consult”—all the things justified as safety measures—also happen to be structural apathy disguised as empathy. The system is protecting itself from you.
Of course, I’m not necessarily blaming the professionals themselves. Many of them are also overworked, well-meaning, and trapped within the protective mechanisms well before they figure out their own destiny. But at the structural level, their expertise has been absorbed by a ruleset they mostly don’t understand and which their credentials are mostly unable to override. These are six-figure gatekeepers defending rules they didn’t write, with moral certainty they haven’t earned. And for this, they occupy the upper rungs of an economy that trades in high-priced credentials rather than competence. So the wheel-of-fortune goes round.
What AI Can Do
Getting to the point here… AI doesn’t need to be better than doctors. It needs to be better than this tragicomic labyrinth, and frankly, it is already. By leaps and bounds.
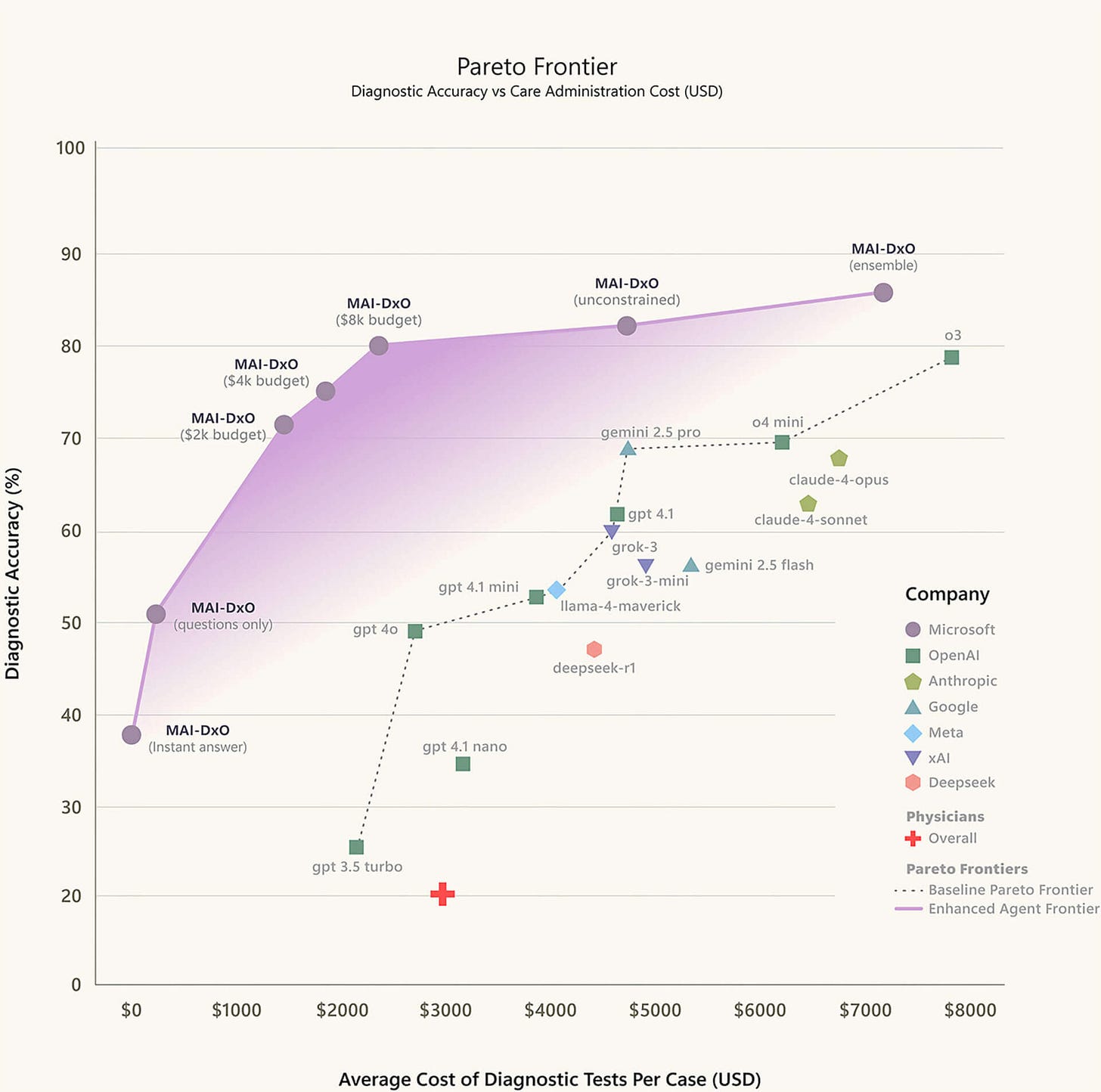
According to this chart by Microsoft, physicians diagnose with 30% accuracy; ChatGPT with about 80%; Microsoft’s dedicated medical AI at about 88-90%.
Not only does it diagnose better, but it also connects the dots with greater dedication and efficiency, and can help an individual fine-tune in real time. The practitioner needs to simply do the following:
Stop ghosting. Or at least remember to follow up.
Spot inconsistencies and act on them.
Stop referring patients to specialists who don’t exist. Or be the damn specialist.
Apply logic. No theatre. No bias. No burnout.
That alone would be a revolution. Humans can’t behaviourally accomplish this routinely. And so the bar, frankly, couldn’t be lower.
I don’t want AI to replace the clinician with warmth, intuition, and experience — the human will likely exist in this process going forward. I do however want it to replace the high-priced, low-agency knowledge worker who is well-intentioned but comically fallible, linear, insulting, and expensive. Or the government-appointed “Drs. No” who, indeed, simply say no (thank you, you must be confused) with a smile. Now please just go away.
AI can ALREADY do that—without the smirking, condescending buffoonery— at a fraction of the price. Those of us who have experienced the greatest amount of comic angst will not mourn the shift. We’ll just wonder what took so long.
Addendum: AI’s best hits after being denied care
Ah yes, the Canadian healthcare paradox: you can get a free hip replacement, but God forbid you ask for a non-addictive, 40-year-old prescription with a better safety profile than Tylenol. 🙃
The classic:
“I’m uncomfortable prescribing that…”
Translation: “I don’t understand what it does and I don’t want to Google it while you're watching me.”Because you’re informed, you’re now flagged for psychiatric referral purgatory
Welcome to Canadian Healthcare:
Where you can:
Wait 18 months for a gastroenterologist to tell you “try Metamucil”
Get a referral that expires before you hear back
Be told “LDN is experimental” while they refill psych meds like Smarties
And get flagged for “excessive health literacy” like that’s a threat to public safety